Chromosomal Scores Unlock Personalized Immunotherapy
Understanding Tumor Aneuploidy and Its Role in Immunotherapy Resistance
Recent research published in Nature Genetics has brought new insights into the challenges of immunotherapy, particularly its limited effectiveness in many cancer patients. Scientists from the University of Chicago have identified tumor aneuploidy—a condition where cells have an abnormal number of chromosomes—as a significant biomarker linked to resistance against immunotherapy across various cancer types. This discovery could reshape how treatments are selected and personalized for patients.
Immunotherapy has revolutionized cancer care, but it still fails in the majority of cases. According to recent studies, between 80% and 90% of patients do not respond effectively to immunotherapy, highlighting the urgent need for better patient selection and improved therapeutic strategies. Researchers are now exploring combinations of therapies that may enhance treatment outcomes, such as the integration of radiation therapy with immunotherapy.
The Impact of Aneuploidy on Treatment Response
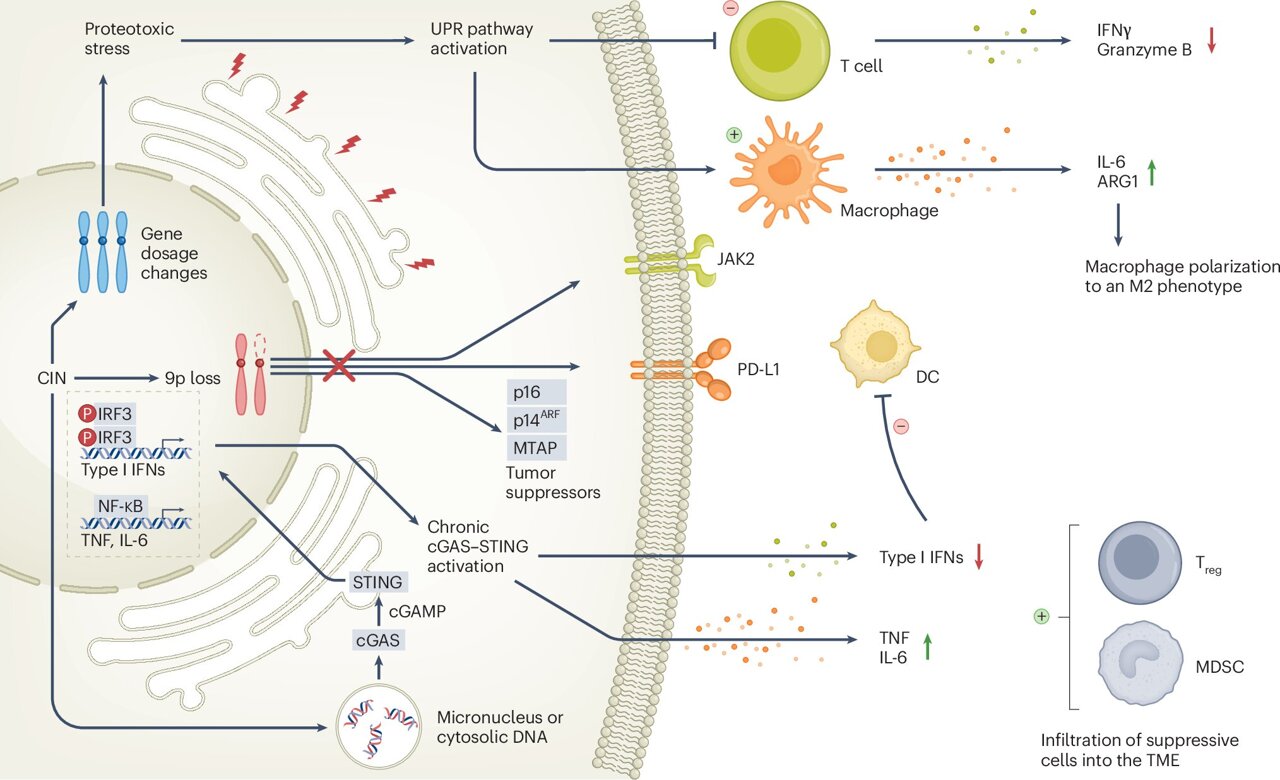
Aneuploidy has long been recognized as a key factor in cancer progression. However, this study expands on previous findings by showing how aneuploidy influences immune evasion and resistance to immunotherapy. Sean Pitroda, MD, Associate Professor of Radiation and Cellular Oncology at UChicago Medicine, led the research team that investigated how chromosomal abnormalities affect the response to treatment.
The study found that combining radiation therapy with immune checkpoint blockade (ICB) can help overcome resistance caused by high levels of aneuploidy. This suggests that radiation may play a crucial role in reprogramming the tumor microenvironment, potentially reducing the presence of immunosuppressive cells and allowing immune cells to target the tumor more effectively.
Combination Therapy: A New Approach
In 2022, Pitroda and his colleagues published a study in Nature Cancer, analyzing non-small cell lung cancer (NSCLC) patients who received various combination treatments. Their findings revealed that tumors with high aneuploidy were less responsive to immunotherapy alone. However, when stereotactic ablative radiotherapy (SABR) was added, the outcomes significantly improved.
Pitroda explained that radiation might work by releasing damage-associated molecular patterns and other signals that stimulate the immune system. This process could make the tumor more visible to the immune system, thereby enhancing the effects of immunotherapy. Although the current recommendations are based on NSCLC, emerging evidence suggests that aneuploidy also affects immunotherapy responses in melanoma, gastrointestinal cancers, and renal cell carcinoma.
Aneuploidy as a Clinical Tool
To translate these findings into practical applications, researchers propose using aneuploidy scores to predict treatment responses and determine which patients would benefit most from adding radiation to their immunotherapy regimen. Advanced tools such as next-generation sequencing and copy number alteration metrics are being used to quantify aneuploidy accurately.
The study emphasizes integrating aneuploidy scores into routine clinical testing alongside existing biomarkers like tumor mutational burden (TMB) and PD-L1 expression. This approach could improve patient selection and guide treatment plans. Notably, aneuploidy and TMB are independent yet complementary, especially in patients with low TMB.
Future Implications and Research Directions
The researchers are working to integrate aneuploidy scores into clinical genomic sequencing platforms to support precision oncology efforts. They also highlight that while many researchers are developing therapies targeting aneuploidy, the challenge lies in the variability of chromosomal alterations among different tumors.
Pitroda notes that future drug development could focus on specific tumors where aneuploidy is more predictable. This could lead to more targeted and effective treatments. The study concludes that tumor aneuploidy is a powerful prognostic and predictive biomarker that can help identify patients most likely to benefit from immunotherapy.
With ongoing research and advancements in technology, the integration of aneuploidy into clinical practice holds great promise for improving cancer treatment outcomes. As scientists continue to explore the mechanisms behind aneuploidy and its impact on immunotherapy, the potential for personalized and more effective cancer care grows stronger.
Post a Comment for "Chromosomal Scores Unlock Personalized Immunotherapy"
Post a Comment