Health Insurers Vow to Overhaul 'Broken' Prior Authorization System
WASHINGTON - After meeting with the nation's top health officials, a consortium of health insurers has promised to take steps to streamline and improve the prior authorization process for plans covering nearly eight out of 10 Americans.
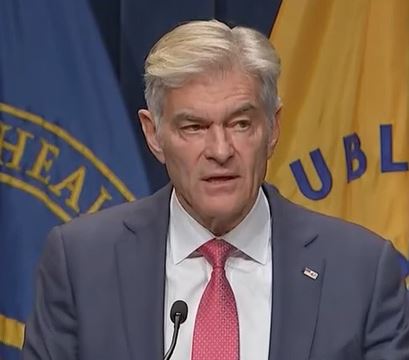
The announcement on Monday by Dr. Mehmet Oz, administrator of the Centers for Medicare and Medicaid Services, and Health Secretary Robert F. Kennedy Jr., came after a roundtable discussion with insurers.
It focused on cutting red tape, accelerating care decisions and enhancing transparency for patients and health care providers interacting with Medicare Advantage, Medicaid Managed Care, Health Insurance Marketplace® and commercial plans.
In addition to federal officials, those participating in the roundtable included representatives of Aetna, Inc., AHIP, Blue Cross Blue Shield Association, CareFirst BlueCross BlueShield, Centene Corporation, The Cigna Group, Elevance Health, GuideWell, Highmark Health, Humana, Inc., Kaiser Permanente and UnitedHealthcare.
"The pledge we're talking about today is not a mandate, not a bill or a rule. And it's not something being legislated," Oz said during a briefing with reporters Monday afternoon.
"Nevertheless, these commitments represent a step in the right direction toward restoring trust, easing burdens on providers, and helping patients receive timely, evidence-based care," he said.
"This is an opportunity for industry to show itself, and the response has been overwhelmingly gratifying" Oz continued.
He said the roundtable and its outcome are also emblematic of a new approach to problem solving at the Department of Health and Human Services and its agencies.
"The effort is being led by wonderful people who realize that there's an opportunity to do good here and that the government doesn't always have to try to do that good itself," Oz said.
"This effort took place with the government as a sponsor, a steward, and as a cheerleader," he said. "It is a lesson in the use of power to convene and to pull together powerful interests."
"The bottom line is, we would like to have private solutions when they’re feasible," he added.
Prior to his remarks, Oz took an informal poll of the room, asking how many in attendance had an issue with pre-authorization affecting their own families.
Judging from the raised hands before him he said the response was reflective of the national average.
"Sadly, 85% of Americans say they've had an experience with pre-authorization that they wished they hadn't. According to the data we have for the Medicare and Medicare Advantage programs in 2023, 3.2 million claims for prior authorization were either partially or fully denied," he said.
What the coalition of private health insurance companies have voluntarily pledged to do is:
- Standardize electronic prior authorization submissions using Fast Healthcare Interoperability Resources®-based application programming interfaces.
- Reduce the volume of medical services subject to prior authorization by Jan. 1, 2026.
- Honor existing authorizations during insurance transitions to ensure continuity of care.
- Enhance transparency and communication around authorization decisions and appeals.
- Expand real-time responses to minimize delays in care with real-time approvals for most requests by 2027, and
- Ensure medical professionals review all clinical denials.
Oz said the Centers for Medicare and Medicaid Services will publish a full list of participating plans later this summer, with details on how the follow-through to the announced commitments are going to roll out.
The hope is that by the end of the calendar year the prior authorization process will be significantly better for health care providers and patients.
"It's a fast timeline, but in seven months, we believe we'll be able to give the American people something they’ve been asking for, and something that’s been in the news recently because it’s been so difficult to get - freedom from prior authorization that's been used incorrectly," Oz said.
He also stressed that the voluntary commitments by the insurers are just the first steps toward "a much larger opportunity."
"This is getting everyone together to focus on a pain point, a thorn in everyone's side, a pebble in our shoes," Oz said. "But the real opportunity is to use this as the first and very important step in building a larger blueprint [for reform].
"It's not just about prior authorization. It’s a template for administrative simplification, to take the paperwork out of the process, and of placing what's good for patients over paperwork," he said.
Dan can be reached at dan@The News Pulse and on X @DanMcCue
The post Health Insurers Pledge to Fix ‘Broken' Prior Authorization System appeared first on The Well News | Pragmatic, Governance, Fiscally Responsible, News & Analysis .
Post a Comment for "Health Insurers Vow to Overhaul 'Broken' Prior Authorization System"
Post a Comment