Rapid Genetic Test Transforms Brain Tumor Diagnosis in the UK
Researchers and medical professionals have created a highly efficient technique for genetic diagnosis of brain tumours. This new approach can reduce the time needed for classification from 6-8 weeks to approximately two hours, potentially enhancing treatment for numerous patients annually across the UK.
The innovative technique, outlined in a new study released today in Neuro-Oncology, has been created by researchers from the University of Nottingham together with doctors at the Nottingham University Hospitals NHS Trust (NUH).
In their published research, the group at NUH employed this innovative method in 50 neurosurgery procedures for brain tumors to achieve swift, real-time diagnostics. The technique boasts a perfect accuracy record, delivering diagnostic outcomes in less than two hours post-surgery and comprehensive tumor categorizations mere moments after sequencing. Additionally, the system’s ongoing sequencing capability ensures an entirely integrated diagnosis can be completed within one day.
Every day in the UK 34 people are diagnosed with some form of brain tumor, equating to more than 12,000 cases a year. The average survival rate can be less than a year for the most aggressive brain cancers.
Brain tumors require complex genetic tests to diagnose, which clinicians currently have to send away to centralised analysis facilities. It can take 6-8 weeks or more to get full results to be able to inform patients what type of tumor they have and their prognosis. This long wait is extremely traumatic for patients, and also delays the start of radiotherapy and chemotherapy which may reduce the chances of treatment working.
The specialists based in Nottingham have created an extremely fast technique for genetic diagnosis of brain tumours, which will remove this lag time. This approach is sufficiently swift that results could be obtained in just a few hours and might enable surgeons to access this data during the procedure itself, thus aiding their decisions about surgery.
Dr. Stuart Smith is a neurosurgeon affiliated with the School of Medicine at the university and also connected to NUH.
He stated: "Historically, identifying brain tumours was a sluggish and costly procedure. With this innovative technology, however, we can offer better support to our patients since they receive their results far quicker—within just two hours—which significantly impacts clinical decisions. Waiting months for these outcomes often heightens patient stress during an already challenging period."
This kind of procedure may take considerable time, thus it’s possible for a surgeon to receive the precise diagnosis mid-operation, influencing their surgical approach accordingly.
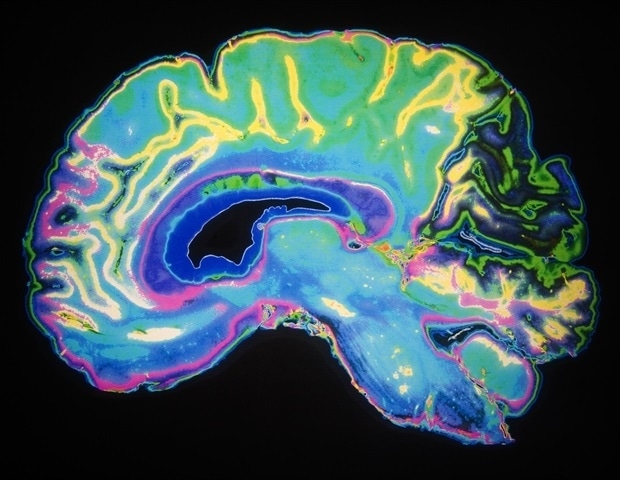
The present treatment process begins with an MRI scan to confirm the existence of a tumour. Following this, patients consult healthcare professionals who outline potential tumour types. In numerous cases, individuals subsequently go through surgical procedures to extract samples from these growths. These tissue specimens are then dispatched to centralized laboratories where tests examine their genetic makeup for anomalies—this analysis ultimately identifies the specific kind of tumour involved.
Historically, specialists would examine the samples directly and adopt a neuropathological approach aimed at recognizing the cells through visual inspection. However, over recent years, this method has evolved with tumors now classified based on their DNA and genetic irregularities—a procedure that was once sluggish because of technical constraints.
Professor Matt Loose, a biologist affiliated with the School of Life Sciences at the University of Nottingham, has devised a technique for targeting particular segments of human DNA with greater precision using portable sequencing devices from Oxford Nanopore Technologies. This approach enables faster examination of significant portions of the human genetic code and facilitates simultaneous analysis of several DNA sections, thus accelerating the overall procedure.
The team has now employed this technique to conduct genetic testing on brain tumor specimens.
ROBIN, a software tool designed for use with P2 PromethION nanopore sequencers, determines DNA sequences by monitoring alterations in electrical currents when individual DNA strands traverse a nanopore—a minuscule aperture—in a membrane.
Professor Loose stated: “Back in 2018, sequencing an entire human genome required approximately five laboratories and spanned half a year, which clearly falls short when swift action is crucial for a patient’s care. However, this novel approach enables us to selectively focus on particular segments of DNA necessary to address precise issues—such as identifying the kind of tumour and determining appropriate treatments. Building upon subsequent studies wherein we enhanced our capability to rapidly examine pertinent sections of the human genome—we currently possess a protocol leveraging ROBIN technology to swiftly generate thorough categorisations of tumours.”
"Once we have a sample from a patient, we can now quickly extract the DNA and look at the different properties to give us the information we need. Methylation is the one we are most interested in early on in this instance because that defines the tumor type."
After a specimen is taken out during the operation, it gets transferred to the pathology laboratory for DNA extraction prior to being dispatched to the sequencing team.
This novel approach to identifying brain tumours is set to be transformative; it’s truly groundbreaking. Not only does it expedite the availability of test outcomes, but the precision of these diagnoses is also remarkably enhanced.
Dr. Simon Paine, Consultant Neuropathologist at NUH
The team are now looking to get the new testing rolled out at NHS Trusts across the UK.
"Not only is the test more accurate and quicker, but it is also cheaper than current methods," said Professor Loose. "Our calculations stand at around £450 per person, potentially less when scaled-up. There are a few reasons for this. Our method can eliminate the need for four to five separate tests, reducing costs as a consequence as we are getting more information from the single test we do. Most importantly, it delivers results to the patients when they need them."
Dr Simon Newman, Chief Scientific Officer at The Brain tumor Charity, said: "The delivery of an accurate diagnosis within hours of surgery will be transformative for all patients ensuring rapid access to the optimal standard of care and - crucially - removing the uncertainty patients face when having to wait weeks for their diagnosis and prognosis.
The capability to merge numerous individual tests into a single procedure and provide them locally represents a transformative step in ensuring equal access to swift and precise molecular diagnostics. The BRAIN MATRIX Trial, supported by the Brain Tumour Charity, is currently investigating how this technology can connect patients with tailored clinical trials throughout the UK.
Patient
Charles Trigg is 45 and from Leicestershire. He was diagnosed with a stage 4 aggressive glioblastoma in April. The results of his genetic tests, which help to assess how sensitive the tumor will be to chemotherapy, to give him a more accurate prognosis, and to allow access to clinical trials in the future are crucial.
The current waiting time on these results is around 8 weeks. This new method has reduced this wait to a week.
Charles said: "From my point of view – to have knowledge is power and it could be the worst knowledge you have, but it gives you certainty and having that certainty actually makes life a hell of a lot easier.
The ability to retrieve data swiftly, enabling a large group of individuals to perform thorough examinations, seems like a remarkable fusion of scientific and medical expertise.
"The pace is phenomenal, and it gives you that certainty and clarity, regardless of whether you like the information, I can't change the information, but what I can do, is take the information I've been given early - and absorb it, feel it and start to plan for the next stage.
Should I possess it? Definitely not! Is it something anyone should have? Absolutely not! Yet, having that comprehension and insight undoubtedly eases the experience considerably compared to being unaware.
University of Nottingham
Deacon, S., et al . (2025). ROBIN: A unified nanopore-based assay integrating intraoperative methylome classification and next-day comprehensive profiling for ultra-rapid tumor diagnosis. Neuro-Oncology . doi.org/10.1093/neuonc/noaf103 .
Post a Comment for "Rapid Genetic Test Transforms Brain Tumor Diagnosis in the UK"
Post a Comment