Deadly Bug Killing Up to 20% of Infected Patients Blamed on Hospital 'Corridor Care'
- READ MORE: Warning as potentially deadly flu-like illness reaches UK shores within 24 hours
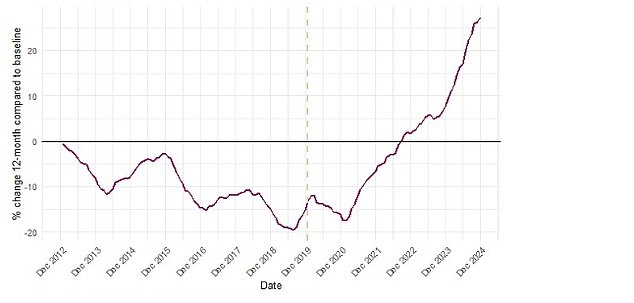
Health officials have cautioned that cases of a deadly hospital-acquired infection, which can rapidly proliferate in medical settings, have risen by approximately one-third over the past year.
Clostridioides difficile, often known as C. diff, is a highly infectious bacterium that leads to diarrhoea.
Although generally mild for many individuals, it can lead to severe complications and has a fatality rate of up to one in every five patients who contract it.
In a recent report, the UK Health Security Agency (UKHSA) stated that the incidence rate observed during 2023-24 stood at 29.5 cases per 100,000 individuals.
This represents a 33 percent increase from 2020-21 and marks the highest point observed in more than ten years, according to the organization.
C. diff is regarded as the primary source of healthcare-associated infections, which occur when a patient is admitted to a hospital.
The bacterium, which first infects the intestine, shows high resistance to both heat and most disinfectant products.
Based on the latest UKHSA report, the overburdened National Health Service might be responsible for the concerning spike.

The agency stated that corridor care – the act of attending to patients in hallways due to insufficient bed availability – might result in overburdened staff failing to adhere to infection prevention control measures.
'Since corridor care takes place when the system is strained, it is logical to infer challenges with IPC adherence, not just because of overburdened healthcare staff but also because resources essential for IPC like handwash sinks may not be easily available outside clinical spaces,' they noted.
Furthermore, the cleaning standards for non-clinical spaces like corridors are not as rigorous as those for clinical areas.
This, coupled with the busy environment of Accident & Emergency departments, might turn these places into possible breeding grounds for C. diff infections.
The agency attributed the increase in C. diff infections to the introduction of corridor care, which is now being studied further.
Routine corridor care has become such a standard practice in certain areas of the NHS that some hospitals are now starting to hire additional staff as a result. dedicated 'corridor medics' to staff these areas.
And a damming report Earlier this year, research conducted by the Royal College of Physicians revealed that four out of every five hospital medical staff were compelled to attend to patients in 'inadequate' public areas.
A physician mentioned that a patient passed away because they were located at an excessive distance from the vital medical apparatus.
According to recent NHS statistics for March, one out of every three accident and emergency patients in England had to wait a minimum of four hours before being attended to.
According to estimates from the Royal College of Emergency Medicine, over 1.5 million patients had to endure waiting times of at least 12 hours for treatment in 2023.
The UK Health Security Agency noted that the significant surge in treatment waitlists following the Covid-19 pandemic might also be playing a role in this increase.
By the conclusion of the previous year, the count of individuals awaiting non-urgent treatment in England reached 7.5 million.
Although this represents a decline from the high point of 7.7 million in September 2023, it remains approximately two-thirds greater than the figures seen back in 2020.
The UK Health Security Agency stated that individuals who have lengthy waits before receiving treatment are at an increased risk of needing antibiotics, which might make them susceptible to Clostridioides difficile infections.
Antibiotics may lead to a disruption in the balance of bacteria typically residing in the gut, thereby raising the likelihood of a C. difficile infection.
The issue turns into a severe health risk if the bacteria spread to other areas of the body beyond the intestines.
This can trigger sepsis, a life-threatening over-reaction from the immune system to an infection.
A further possible complication involves bacteria leaking into other regions of the abdominal cavity, leading to a life-threatening infection known as peritonitis.
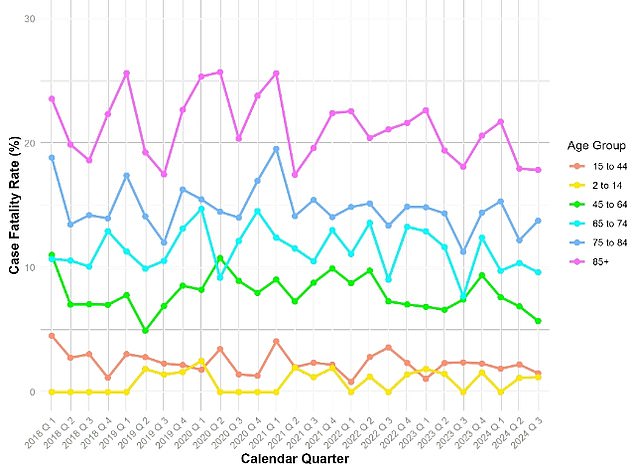
New figures from UKHSA indicate that mortality rates for C. diff infections were most severe among those aged 85 and older, reaching almost 20 percent.
The fatality rate reduced as age increased, showing that individuals aged 45 to 64 had merely a 5 percent probability of succumbing to the condition.
UKHSA stated that 'not only have the rates of C.diff risen consistently since 2020, but also the pace at which these figures are increasing has sped up.'
The body further stated that although hospitals were responsible for the largest share of C. diff infections, there had also been an observed rise in such cases within the community.
C. diff spreads through spores present in the feces of infected individuals, which can remain viable in the surroundings for extended periods.
This enables their transmission through individuals who have come into contact with those sickened patients or touched contaminated surfaces.
The symptoms of a C. diff infection encompass diarrhoea, fever, lack of appetite, queasiness, and abdominal discomfort.
Individuals who have experienced diarrhoea and have recently been prescribed antibiotics, noticed blood in their stool, or suffered from persistent diarrhoea lasting seven days or longer should reach out to NHS 111 or their general practitioner for guidance.
Read more
Post a Comment for "Deadly Bug Killing Up to 20% of Infected Patients Blamed on Hospital 'Corridor Care'"
Post a Comment